20 yr girl with b/l pedal edema
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
A pavan kumar
1701006011
Presentation
20 year female came to casualty with chief complaints of
-Hyperpigmented macules since 15 days
-b/l pedal edema since 15 days
Fever 15 days back
-abdominal distension since 8 days
-cough(dry) since 7 days
-Sore throat since 7 days
-decreased appetite since 7 days
-decreased urine output since 3 days
-constipation since 3 days
-SOB since 5 days
HOPI
20 year old female came with c/o of b/l pitting type pedal edema extending till knees since 15 days to which she got medical health checkup and prescribed some medication (unknown) then her pedal edema got resolved along with fever she developed Hyperpigmented macules on face later they stopped medications after 2 days she again had a complaints of b/l pedal edema and fever abdominal distension associated with dry cough and decreased appetite she also has a complaints of DECREASED urine output and constipation since 3 days passing stools once in 3 to 4 days
N/k/c/o HTN DM THYROID DISORDER CAD EPILEPSY TB
Personal history:
Mixed diet
Appetite lost
Non veg diet
Bowel and bladder movements are decreased
Family history :
No significant family history
O/E :
Pt was c/c/c
On admission vitals are
Bp 110/70
PR 79
RR 19
Temp 98.8
CVS- apex beat replaced laterally palpable thrills and s1 s2 heard mild s3
RS - BAE decreased rt infra scapular crepts present
P/a umblicus is everted
CNS
MMSE
https://youtube.com/shorts/9YYfuCgbNl8?feature=share
https://youtube.com/shorts/ZN8AZcvPjYs?feature=share
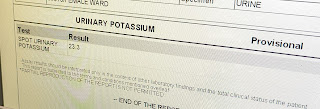
Investigations:
28/09/22
29/9/22
ICU BED NO. 2
S
B/l pedal edema SOB
Fever spikes
O
Pt c/c/c
Bp - 120/70
PR - 142
RR- 29
Temp-99.5
Spo2 - 94 at room air
A
Post streptococcal glomerulonephritis..??
IGA nephropathy..??
Infective endocarditis..??
P
1)INJ Augmentin 1.2gm iv BD
2)INJ lasix 40mg iv BD
3) NEB Duolin, Budocort 6th hourly
4) INJ neomol 1gm/iv/sos
5) TAB Azithromycin 500mg po bd
6) Betadine gargles tid
30/9/22
ICU BED NO. 2
S
Fever spikes +
Stools not passed
O
Pt c/c/c
Bp - 1110/70
PR - 128
RR- 29
Temp-100.6
Spo2 - 94 at room air
A
Post streptococcal glomerulonephritis..??
IGA nephropathy..??
Infective endocarditis..??
Polyserositis 2' to SLE
P
1)INJ Augmentin 1.2gm iv BD
2)INJ lasix 40mg iv BD
3) NEB Duolin, Budocort 6th hourly
4) INJ neomol 1gm/iv/sos
5) tab prednisolone 50mg po bd
6) Betadine gargles tid
7) inj pan 40 mg iv bd
1/10/22
ICU BED NO. 2
S
B/l pedal edema subsided
COUGH +
O
Pt c/c/c
Bp - 110/70
PR - 125
RR- 29
Temp-98.6
Spo2 - 94 at room air
A
Falreup of SLE
infective endocarditis
Drug induced
P
1)INJ CEFTRIAXONE 1GM IV BD
2)INJ PAN 40 MG IV OD
3) INJ LASIX 40 MG IV BD
4) INJ DERIPHYLLIN 100MG IV BD
5) INJ NEOMOL 1GM IV SOS
6) TAB PREDNISOLONE 50 MG PO BD
7) NEB BUDECORT 12TH HOURLY
2/10/22
ICU BED NO. 2
S
Action tremors +
FEVER SPIKES +
O
Pt c/c/c
Bp - 120/70
PR - 101
RR- 22
Temp-99.5
Spo2 - 94 at room air
A
FLARE UP SLE WITH
LUPUS NEPHRITIS
CNS LUPUS VASCULITIS
P
1) Iv fluids NS @30ml/hr
2) inj methyl Prednisone 750mg in 100ml NS IV OD
3) INJ. CEFTRIAXONE 1GM IV/BD
4) INJ. PAN 40 MG IV/OD
5) INJ. LASIX 40 MG IV OD
6) INJ.NEOMOL 1GM IV/SOS
7) INJ. DERIPHYLLIN 100MG IV/BD
8) INJ. TRAMADOL 100MG IN 100 ML NS IV/BD
9) TAB HCQ 200 MG PO/OD
10) TAB. PREDNISOLONE 30MG/PO/BD
11) TAB. DOLO 650 MG PO/TID
12) NEB . BUDECORT P/N 12TH HRLY
13) BP, PR, TEMP, 4TH HRLY CHARTING
3/10/22
ICU BED NO. 2
S
B/l pedal edema subsided
COUGH +
Pt c/c/c
Bp - 110/70
PR - 125
RR- 29
Temp-98.6
Spo2 - 94 at room air
A
Falreup of SLE
LUPUS NEPHRITIS
CNS vasculitis
P
1)INJ CEFTRIAXONE 1GM IV BD
2)INJ PAN 40 MG IV OD
3) INJ LASIX 40 MG IV BD
4) INJ DERIPHYLLIN 100MG IV BD
5) INJ NEOMOL 1GM IV SOS
6) TAB PREDNISOLONE 50 MG PO BD
7) NEB BUDECORT 12TH HOURLYSolved
8) IV fluids NS @50 ml/hr
9) inj methyl Prednisone IV OD
10) tab hcq200mg po od
11) oint t bact l/a bd
12) neosporin powder for l/a
4/10/22
ICU BED NO. 2
S
B/l pedal edema subsided
COUGH +
Pt c/c/c
Bp - 110/70
PR - 125
RR- 29
Temp-98.6
Spo2 - 94 at room air
A
Falreup of SLE
LUPUS NEPHRITIS
CNS vasculitis
P
1)INJ CEFTRIAXONE 1GM IV BD
2)INJ PAN 40 MG IV OD
3) INJ LASIX 40 MG IV BD
4) INJ DERIPHYLLIN 100MG IV BD
5) INJ NEOMOL 1GM IV SOS
6) TAB PREDNISOLONE 50 MG PO BD
7) NEB BUDECORT 12TH HOURLYSolved
8) IV fluids NS @50 ml/hr
9) inj methyl Prednisone IV OD
10) tab hcq200mg po od
11) oint t bact l/a bd
12) neosporin powder for l/a
08/10/22
S
No fever spikes
Pt c/c/c
Bp - 120/90
PR - 74
RR- 16
Temp-98
Spo2 - 98 at room air
A
Falreup of SLE
LUPUS NEPHRITIS
CNS vasculitis
P
1)TAB. PAN 40 MG PO OD
2)TAB. MCQ 200MG/PO/OD
3) TAB PREDNISOLONE 20 MG PO BD
4) TAB. AZORAN 50 MG PO BD
5) TAB. WARFARIN 5MG PO OD
6) TAB. WARFARIN 5MG PO OD
6) SYP. DULPHALAC 15 ML / PO/ TID
7) OINT - T - BACT L/A BD
8) CEBHYDRA LOTION L/A BD
9) NEOSPORIN POWDER L/A


































Comments
Post a Comment